COVID-19 May Cause Accumulation of Alzheimer's-Related Protein Aggregates in Eyes and Brain
In a groundbreaking study published in the journal Science Advances, researchers have discovered a potential link between COVID-19 and the buildup of amyloid-β protein plaques in the central nervous system (CNS), a hallmark associated with Alzheimer's disease. This connection could help explain the mystery behind brain fog in long COVID, a condition affecting many survivors of the virus.
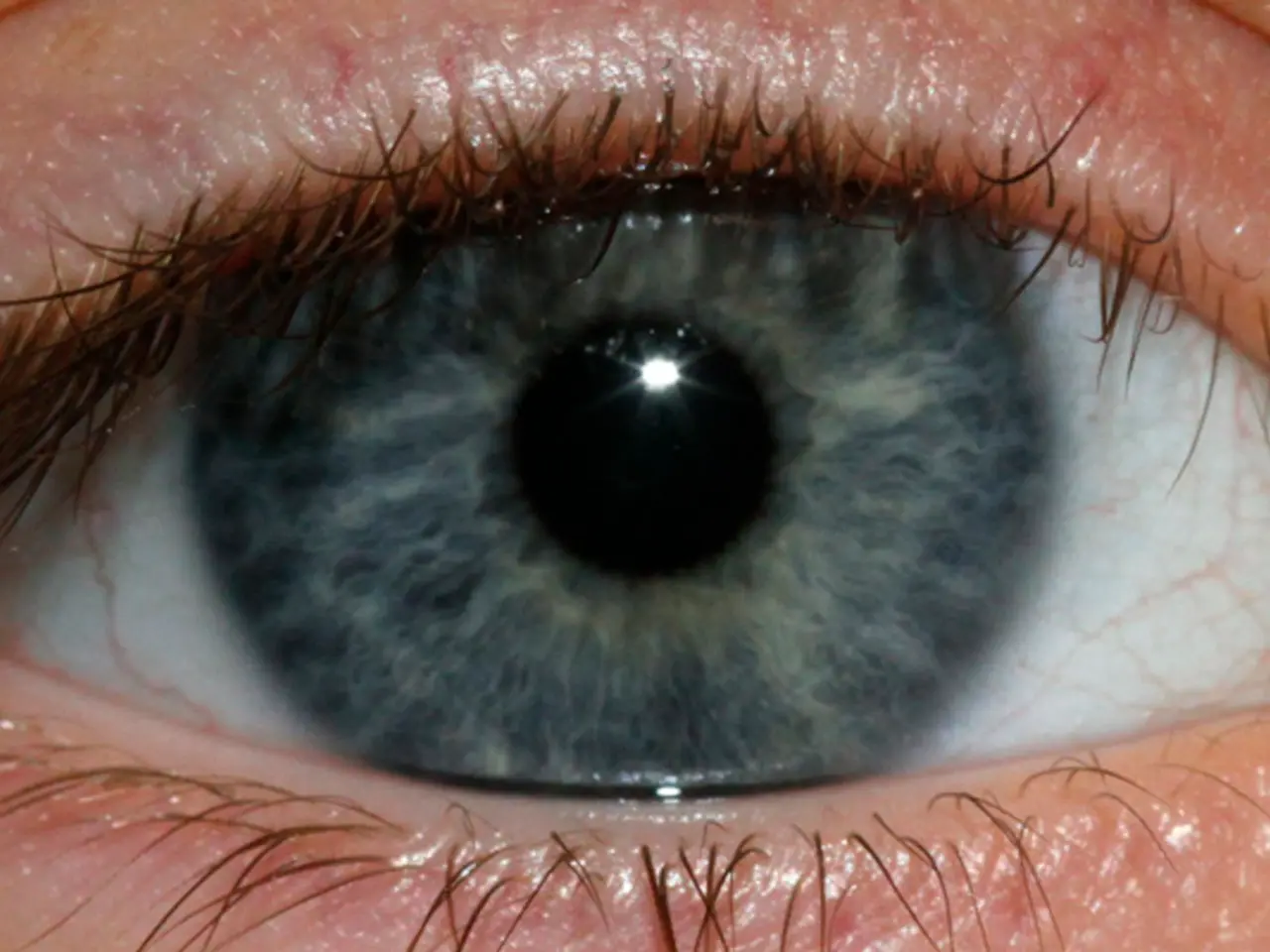
The study, led by Dr. Brian Hafler, MD, PhD, used human retinal "mini-organs" instead of animal models, providing advantages due to the human-specific aspect of the model. These organoids were exposed to COVID-19 spike proteins, resulting in increased amyloid-β levels. Remarkably, higher amyloid-β levels were found in retinal tissues from COVID-19 patients with no history of dementia, similar to Alzheimer's patients.
The SARS-CoV-2 spike 1 protein appears to be the key player in this mechanism. It induces amyloid-β plaque formation by interacting with CNS cells, as shown in the human retinal models where spike protein exposure significantly increased amyloid-β deposition. These plaques colocalize with spike protein in retinal tissue, linking viral protein presence and plaque development.
Amyloid-β may not only be a pathological marker but could play a protective role in the brain's innate immune response, acting as an antimicrobial peptide that aggregates in response to viral infection to help combat it. This suggests that amyloid-β buildup during COVID-19 might reflect an immune defense mechanism triggered by SARS-CoV-2.
The increase in amyloid-β due to COVID-19 may contribute to neurological impairments such as memory and learning deficits, colloquially manifested as brain fog, and potentially raises concerns about heightened long-term Alzheimer's disease risk in COVID-19 survivors.
The study also identifies a potential therapeutic target to mitigate SARS-CoV-2-induced amyloid pathology and its cognitive sequelae. Blocking neuropilin-1 (NRP1), a receptor involved in viral entry and amyloid-β accumulation, reduced plaque formation in experimental settings. This opens up the possibility of NRP1 inhibitors as potential treatments for neurological complications after COVID-19 infection.
It's important to note that the term "brain fog" was reported by people with chronic health conditions such as fibromyalgia and those undergoing menopause before COVID-19. However, the study bolsters the amyloid beta antimicrobial hypothesis of Alzheimer's disease, suggesting that amyloid beta could act as part of the brain's innate immune response against viral infections.
Further research is ongoing to clarify long-term outcomes and develop treatments targeting this pathway. The ultimate goal of the study is to prevent long-term neurological effects of COVID-19 and explore NRP1 inhibitors and other modulators of virus-host interactions as potential therapeutics for preventing viral-induced amyloid pathology and Alzheimer's disease.
Interestingly, NRP1 inhibitors are under investigation as potential anticancer drugs, adding another layer of complexity to their potential therapeutic applications. Alzheimer's disease is associated with two major proteins, amyloid-β and tau, and further research is needed to understand the interplay between these proteins and the SARS-CoV-2 spike protein in the development of neurological complications after COVID-19 infection.
In conclusion, the study provides compelling evidence that COVID-19 infection can promote amyloid-β plaque formation in CNS tissues, contributing to cognitive symptoms including brain fog and potentially increasing Alzheimer's disease risk. The study's findings could have significant implications for understanding and treating long COVID and its neurological effects.
- This study published in Science Advances on COVID-19 and amyloid-β protein plaques in the CNS raises concerns about a potential long-term Alzheimer's disease risk in COVID-19 survivors.
- The researchers used human retinal "mini-organs" to discover a connection between COVID-19 and amyloid-β plaque buildup in the brain, which could partially explain brain fog in long COVID.
- The SARS-CoV-2 spike 1 protein appears to induce amyloid-β plaque formation by interacting with CNS cells, a process that could lead to memory and learning deficits, colloquially known as brain fog.
- The study identifies blocking neuropilin-1 (NRP1) as a potential therapeutic target to mitigate SARS-CoV-2-induced amyloid pathology and its cognitive sequelae, such as neurological complications after COVID-19 infection.
- Interestingly, NRP1 inhibitors, under investigation as potential anticancer drugs, could also be applicable in treating long-term neurological effects of COVID-19.
- Further research is essential to uncover long-term outcomes, develop treatments targeting this pathway, and better understand the interplay between amyloid-β, tau proteins, and the SARS-CoV-2 spike protein in the development of neurological complications after COVID-19 infection.