Rheumatoid Arthritis and the ACPA Link: Essential Information Explored
Revamped Article:
Rheumatoid Arthritis (RA) and Anti-Citrullinated Protein Antibodies (ACPAs): A Closer Look
A battle within the body occurs when ACPAs are produced by the immune system, targeting citrullinated proteins. This intricate dance is a crucial part of RA diagnosis and prognosis.
RA is an autoimmune condition, meaning that the body's defense system mistakes its own tissues for foreign invaders, leading to painful inflammation in the joints. And one of the weapons in its arsenal is ACPAs that disrupt specific cell processes, driving a vicious cycle of damage and further immune system activity.
ACPAs: Warning Sign or Harmless Byproduct?
A 2021 literature review reveals that ACPAs act as a specific biological sign, or biomarker, in the blood, indicating RA. Yet, a positive ACPA test doesn't necessarily mean a person has RA. The presence of rheumatoid factor (RF), another antibody, may also be an indicator of the condition.
Doctors will evaluate both antibodies during RA diagnosis, as they provide valuable insights into disease progression and outlook. For example, an individual with a positive ACPA and RF tests might have more severe RA symptoms. Conversely, someone with only a positive ACPA test may exhibit early RA symptoms or have a future risk of developing the condition.
Intriguingly, if both ACPA and RF tests are negative, a person may still have RA, based on other symptoms, or develop ACPAs over time. Moreover, a positive ACPA test doesn't necessarily mean a person has RA, as they might have another autoimmune condition, such as systemic lupus erythematosus (SLE) or Sjögren disease.
ACPA-Positive or ACPA-Negative RA: Differing Impact?
The presence or absence of ACPAs can impact RA progression and response to treatment.
A 2022 study found that people with ACPA-positive RA experienced continuous joint inflammation during remission periods. In contrast, those with ACPA-negative RA responded more significantly to disease-modifying antirheumatic drugs (DMARDs) within the first year of therapy.
Interestingly, people with ACPA-negative RA in remission appear to have inflammation levels comparable to those who do not have RA. In contrast, individuals with ACPA-positive RA in remission exhibit substantially lower inflammation levels from the onset of the disease.
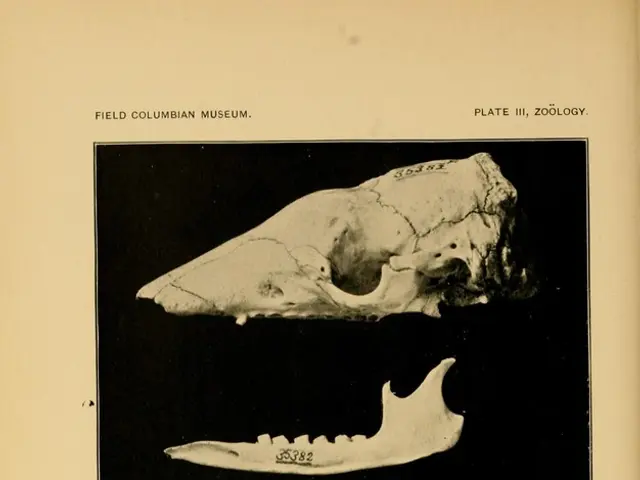
Another 2022 study concluded that ACPA-positive RA patients displayed more severe bone damage than those with ACPA-negative RA, often emerging in the fifth metatarsophalangeal joint, or little toe joint. This erosion tends to occur more frequently and severely in ACPA-positive RA cases.
The Cause of the ACPA Controversy: Citrullination
The immune system aids citrullination, a process where an enzyme called peptidyl-arginine deiminase (PAD) converts arginine, a protein building block, into citrulline. While this process is essential for brain development, skin health, and natural cell death, it intensifies in people with RA. One of the proteins affected is collagen, which plays a crucial role in connective tissue, tendons, and ligaments.
Cell damage may cause PAD to work overtime, resulting in excess citrullination. In response, the immune system creates ACPAs that attack these citrullinated proteins. However, PAD resides in immune cells like neutrophils and monocytes, and ACPAs may reactivate neutrophils, leading to further citrullination. This cycle escalates inflammation and tissue damage in RA patients. Factors such as smoking or air pollution may exacerbate this cycle.
Testing for ACPAs: A Tiny Puncture, Big Implications
Physicians can identify ACPAs with a simple 5-minute blood test for CCP antibodies. This test helps doctors diagnose or rule out RA. However, other conditions can also cause raised CCP antibodies, such as SLE, Sjögren disease, tuberculosis (TB), or chronic lung disease. A doctor will consider additional factors, like a person's medical history, physical examination, and the results of other tests, when diagnosing RA.
"Learn more:How does a doctor diagnose rheumatoid arthritis?## Additional RA Diagnostic Tests
Besides the CCP antibody test, doctors may test for other biomarkers when confirming RA. These include antinuclear antibodies, C-reactive protein, RF, synovial fluid analysis, and X-rays of the joints to assess damage.
ACPA vs. CCP Antibodies: What's the Difference?
According to a 2022 review, anti-cyclic citrullinated peptides (anti-CCP) antibodies are a type of ACPA that reacts to specific CCPs like fibrinogen or myelin basic protein. While ACPAs can react to a broader range of proteins, anti-CCP antibodies display a specific response to each CCP.
"Learn more:Anti-CCP testing for rheumatoid arthritis## The Bottom Line
In conclusion, ACPAs are integral to RA diagnosis and prognosis. By understanding the differences between ACPA-positive and ACPA-negative RA, doctors can tailor treatment plans to achieve optimal outcomes. Future research is needed to further delve into the complex interplay between ACPAs, the immune system, and RA development and progression.
- The production of ACPAs by the immune system leads to the targeting of citrullinated proteins, a crucial part of Rheumatoid Arthritis (RA) diagnosis and prognosis.
- ACPAs serve as specific biological signs or biomarkers, indicating RA, according to a 2021 literature review, but a positive ACPA test doesn't necessarily mean a person has RA.
- Doctors consider both ACPAs and rheumatoid factor (RF) during RA diagnosis, as they offer valuable insights into disease progression and outlook.
- People with ACPA-positive RA may experience continuous joint inflammation during remission periods, while those with ACPA-negative RA respond more significantly to disease-modifying antirheumatic drugs (DMARDs) within the first year of therapy.
- ACPA-positive RA patients tend to display more severe bone damage than those with ACPA-negative RA, as shown by a 2022 study.
- The immune system aids citrullination, a process where an enzyme converts arginine into citrulline, intensifying in people with RA. This process may exacerbate the cycle of ACPA production and tissue damage.
- Physicians can identify ACPAs with a simple 5-minute blood test for CCP antibodies, a crucial tool for diagnosing or ruling out RA, but other conditions can also cause raised CCP antibodies.